Search
Recent comments
- google bias...
6 hours 5 min ago - other games....
6 hours 8 min ago - נקמה (revenge)....
7 hours 8 min ago - "the west won!"....
9 hours 12 min ago - wagenknecht......
9 hours 53 min ago - the game of war....
12 hours 17 min ago - three packages....
13 hours 37 min ago - russian oil.....
13 hours 44 min ago - crime against peace....
21 hours 56 min ago - why is Germany supporting the ukrainian nazis?....
23 hours 9 min ago
Democracy Links
Member's Off-site Blogs
a gut feeling about why your social life stinks...
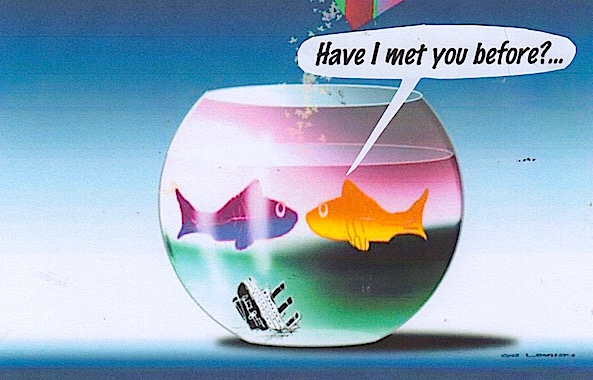 Accumulating evidence suggests that the microbiota living in and on animals has important functions in the social architecture of those animals. Sherwin et al. review how the microbiota might facilitate neurodevelopment, help program social behaviors, and facilitate communication in various animal species, including humans.
Accumulating evidence suggests that the microbiota living in and on animals has important functions in the social architecture of those animals. Sherwin et al. review how the microbiota might facilitate neurodevelopment, help program social behaviors, and facilitate communication in various animal species, including humans.
Understanding the complex relationship between microbiota and animal sociability may also identify avenues for treating social disorders in humans.
Increasingly, it is recognized that the microbes resident in the gastrointestinal tract can influence brain physiology and behavior. Research has shown that the gastrointestinal microbiota can signal to the brain via a diverse set of pathways, including immune activation, production of microbial metabolites and peptides, activation of the vagus nerve, and production of various neurotransmitters and neuromodulators in the gut itself. Collectively, this bidirectional pathway is known as the microbiota-gut-brain axis. In the absence of a microbiota, germ-free and antibiotic-treated mice exhibit alterations to several central physiological processes such as neurotransmitter turnover, neuroinflammation, neurogenesis, and neuronal morphology. Perhaps as a result of these neurological alterations, the behavior of rodents lacking a microbiota—especially social behavior—is remarkably different from that of rodents colonized with bacteria. Conversely, supplementation of animals with certain beneficial live bacteria (e.g., Bifidobacterium and Lactobacillus) can lead to notable improvements in social behavior both in early life and in adulthood. Collectively, these results suggest that microbial signals are important for healthy neurodevelopment and programming of social behaviors in the brain. Although research on the functional and ecological implications of the gut microbiota in natural populations is growing, from an evolutionary perspective it remains unclear why and when relationships between microbes and the social brain arose. We propose that a trans-species analysis may aid in our understanding of human sociability.
Read more:
Eoin Sherwin1, Seth R. Bordenstein2, John L. Quinn3, Timothy G. Dinan1,4, John F. Cryan1,5,*
Science 01 Nov 2019:
Vol. 366, Issue 6465, eaar2016
- By Gus Leonisky at 27 Nov 2019 - 6:55am
- Gus Leonisky's blog
- Login or register to post comments
explaining the rise in modern health diseases...
From hunter-gathering to industrialization, our gut microbiome has adapted and evolved under environmental pressures. The current period of modernization is seeing changes in dietary patterns and medical practices that have driven a deterioration of gut microbial communities over generations. And this, in turn, contributes to explaining the current rise in chronic diseases in industrialized societies.
A new opinion article from Erica D. Sonnenburg and Justin L. Sonnenburg from the Stanford University School of Medicine explores the implications for human health of the changes related to modern lifestyle that are reflected in the gut microbiome of different populations.
Humans have co-evolved with our microbiota over time. The ancestral human communities who mainly consumed plant-based diets harbored a gut microbiota profile that was well adapted to consuming microbiota-accessible carbohydrates (MACs) and a human genome that had similarly adapted to this microbiota profile.
However, a low-MAC diet and antibiotics secondary to industrialization have led to an altered gut microbiota, with a decrease in species that degrade fibers and an enrichment of mucus-degrading microorganisms and bacterial species that harbor antibiotic-resistant genes. These modern changes in the gut microbiota—called “microbiota insufficiency syndrome” by the authors—can lead to the loss of our ancestral microbial heritage, with any recovery of the microorganisms that have disappeared being highly unlikely.
Several drivers of gut microbiome alterations in modern populations include delivery type, antibiotic use, diet and sanitation. For instance, the effects of a Western-style diet low in MACs on gut bacterial species have been well documented across geographically and culturally diverse human populations, leading to a compositional shift in the gut microbiota that varies depending on the degree of transition from a foraging lifestyle to industrialization. In addition, and even more dramatically, these shifts are still apparent and irreversible over four generations of mice.
Although the genes of the microbiota can easily and rapidly adapt to short-term exposure to an environmental stimulus (e.g. Western diet and the indiscriminate use of antibiotics), the human genome may need several generations to adapt. The authors suggest that this incompatibility may contribute to explaining the rise in modern health diseases, such as inflammation-related conditions and non-communicable chronic diseases. For instance, genes that promote calorie restriction were useful among the nomadic human population where food resources were scarce, but many generations passed before their expression decreased in today’s society, with the rise in obesity-related disorders, as an adjustment of the human genome to the current obesogenic environment.
Read more:
https://www.gutmicrobiotaforhealth.com/en/the-impact-of-industrializatio...
when democracy is influenced by our guts...
Over the past 15 years, researchers have come to appreciate how profoundly the diverse zoo of microbes in the human gut, skin, and mouth affects our health. But their identities and exactly how they exert their effects have remained mysterious. Now, two research groups have made this microbial dark matter more visible, by starting with its best-known aspect: its DNA. One team harnessed DNA sequence information to isolate specific microbes they wanted to grow in lab dishes. The other used it to discover chemicals that microbes make to communicate with each other and influence their human host. By opening the way to a more detailed understanding of the trillions of microbes we contain, the techniques could lead to new treatments.
Read more:
Science 04 Oct 2019:
Vol. 366, Issue 6461, pp. 23
Read from top.